Arcane (Antimicrobial Resistance Control through Adaptive healthcare NEtworks) project
We’ve all heard the term “superbug,” and it sounds like something out of a science fiction movie. But the reality of antimicrobial resistance (AMR) is one of the most significant public health challenges of our time. These are bacteria that have evolved to resist our most powerful antibiotics, making common infections difficult, and sometimes impossible, to treat.
A major frontline in this battle is our healthcare system. When people are at their most vulnerable – sick in a hospital – they are more susceptible to infections. Add in the widespread use of antibiotics in these facilities, and you have a perfect storm for the rise and spread of antibiotic-resistant bacteria.
For the past few years, the intense focus on infection control due to the COVID-19 pandemic gave us a temporary advantage. The masks, the hand sanitizer, the social distancing – all of these measures inadvertently helped to curb the spread of these superbugs. However, the pandemic also brought challenges, such as overwhelmed hospitals and increased antibiotic use in COVID-19 patients, which may have unfortunately counteracted some of those gains.
More Than Just a Hospital: Uncovering the Hidden Network
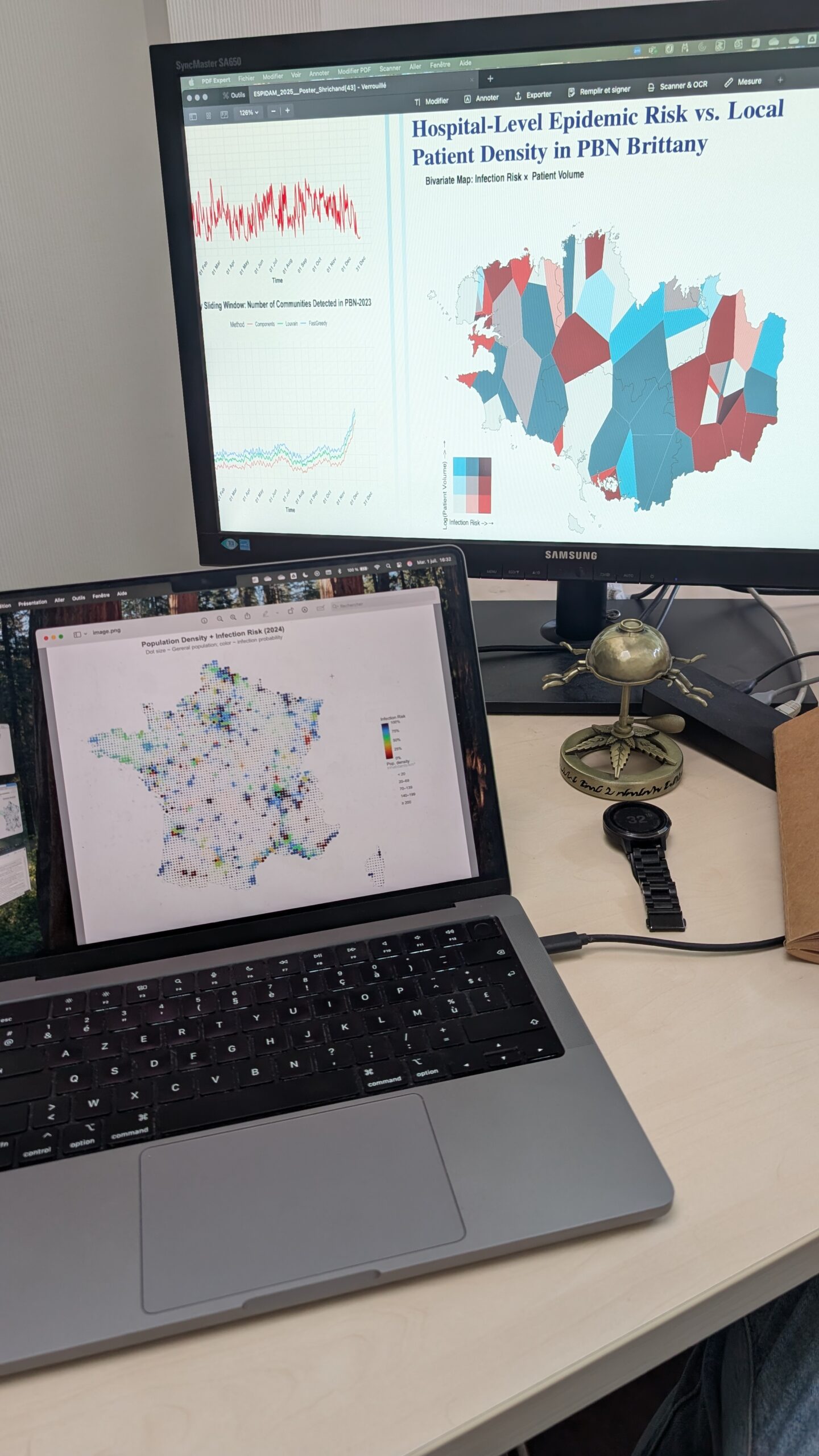
Hospitals don’t exist in a vacuum. They are interconnected hubs, linked by the constant flow of patients and staff. A patient might be transferred from a local clinic to a large university hospital, or a specialist might work across several institutions. This creates a complex, invisible web – a healthcare network.
Our team, along with our collaborators, has been at the forefront of studying these networks. We’ve shown that these connections between healthcare facilities are a critical pathway for the spread of antibiotic-resistant bacteria across a country, and even across borders.
Our Project: Mapping the Spread to Stop the Spread
This brings us to our current project. We want to dig deeper. We aim to understand precisely how the ever-changing nature of these healthcare networks influences the spread of resistant bacteria at local, national, and even international levels.
We’ll be asking questions like:
- How do seasonal changes or unexpected events impact the network and, in turn, the spread of infections?
- What role do specific patient characteristics or the initial “seeding” of a resistant bacteria in a hospital play?
To answer these questions, we’re combining three powerful approaches: analyzing real-world data, creating mathematical models, and running sophisticated computer simulations.
A Tale of Two Countries: France and Germany
To ground our research in the real world, we’ll be focusing on France, Germany, and the border region they share. By comparing and contrasting the healthcare networks and public health protocols in these two countries, we can see how different national strategies impact the spread of AMR. We’re particularly interested in the role of cross-border patient-sharing in the dynamics of these superbugs.
By modeling different control measures – at the hospital, regional, and national levels – we can assess their potential impact over time.
The Bigger Picture: Paving the Way for Smarter Public Health
Ultimately, our goal is to provide actionable insights for public health decision-making. By understanding which control measures are most effective based on the specific characteristics of a healthcare network, we can help policymakers in France, Germany, and beyond to develop more targeted and efficient strategies to protect patients and combat the growing threat of antimicrobial resistance. This research is a crucial step towards a future where we can stay ahead of the superbugs.
Arcane is funded by ANR and DFG (2024-2028)